
Understanding and controlling the threat of Shiga toxin-producing E. coli
17 June 2024 | Gail Betts, Head of Microbiology, and Suzanne Jordan, Molecular Microbiology and Methods Section Lead
E. coli is a common microorganism, widespread in the environment and present in vast numbers in animal and human gut contents – where they are usually harmless.
The presence of ‘generic’ E. coli in foods should be considered as a hygiene indicator and ideally, we would like none to be present, although we may accept very low levels on some food types. Increases in the levels of E. coli in a product (or its associated production environment) would indicate that immediate improvements in hygiene are needed.
Shiga toxin-producing E. coli (STEC) are thought to be the most potent group of pathogenic E. coli, and have been implicated in recent recalls of prepacked, ready-to-eat sandwiches, wraps and salads (June 2024), as well as Lancashire cheese recalls over the 2023 Christmas period.
Controlling Shiga toxin-producing E. coli (STEC) – preventing contamination and recalls
Is your business fully protected?
But what do the terms E. coli, STEC, VTEC, O157 mean? And what is the difference between Shiga toxin-producing E. coli (STEC) and non- Shiga toxin-producing E. coli?
STEC the pathogen
STEC are a group of E. coli that possess stx genes which code for “Shiga toxin” (sometimes referred to as Verocytotoxin). There are many hundreds of STEC serogroups that exist which all have the potential to cause human illness, and E. coli O157 is the most well-known within this group. In addition, some STEC strains are also capable of attaching to the gut wall, resulting in even more severe illness.
Initial cases of Shiga toxin-producing E. coli (STEC) were reported in the early 1980s, with the first outbreaks caused by E. coli belonging to serogroup O157:H7 (abbreviated to E. coli O157). It soon became evident that this organism had a low infective dose. Over the next few years, E. coli serogroups other than O157 were reported to cause similar serious symptoms. This was when the term ‘STEC’, sometimes known as Verocytotoxin-producing E. coli (VTEC) came into use to describe all pathogenic E. coli capable of producing the Shiga toxin.
Significance of STEC
One of the main reasons for concern about STEC is their low infective dose, with the ingestion of just ten cells believed to cause illness. Symptoms caused by STEC microorganisms include severe diarrhoea (including bloody diarrhoea), abdominal pain, and sometimes haemolytic uremic syndrome.
If STEC contaminated food is consumed, the cells can multiply when they reach the gut. STEC strains that can attach to the gut wall may cause haemorrhagic colitis or severe bloody diarrhoea. Other complications can occur if the Shiga toxin produced by STEC enters the bloodstream. Shiga toxin in the blood will potentially cause kidney damage, leading to haemolytic uremic syndrome. These severe symptoms often result in hospitalisation and, in the worst cases, death.
The low infective dose, together with its symptoms, enable the potential spread of STEC between those that are ill and healthy individuals. Great care should be taken with personal hygiene to prevent person-to-person spread.
Non-O157 STEC microorganisms
Although the O157 serogroup remains a major cause of STEC-related illness in many countries, a wide range of other serogroups have been reported to cause serious outbreaks. In response to this, several countries have implemented control measures to analyse for, and prevent the sale of, contaminated products. The control measures often include the analysis of named food types for defined STEC serogroups that are now recognised to have caused, or have the potential to cause, serious illness.
In the USA there is a legal requirement to test various beef cuts for STEC serogroups O26, O45, O103, O111, O121, O145 and O157 referred to as the ‘Top Seven’ STEC. EU legislation requires that manufacturers of sprouted seeds test seeds destined for sprouting or sprouted seed irrigation water for STEC serogroups O157, O26, O103, O111, O145 and O104:H4 known as ‘Top Six’ STEC. Any products reported to have STEC present may not be placed on the market.
Our views on STEC are changing as the reliance we have on specific pathogenic serogroups is challenged. Future changes will shift the focus from named serogroups thought to be highly pathogenic, to the presence of any STEC as a major safety risk.
Food and drink products at risk of STEC contamination
Many of the initial E. coli O157 outbreaks in the late 1980s were caused by improperly handled or undercooked beef and beef products. Since then, O157 outbreaks have been associated with several foods, including raw milk and dairy products, various cooked meats, fruits (e.g. apples), vegetables (e.g. spinach), salads (e.g. lettuce, watercress), nuts and sprouted seeds.
The main source of STEC contamination of foods originates from a primary animal source (the animal gut). Milk and dairy products can be contaminated through poor dairy hygiene during milking; raw meats as a result of poor abattoir hygiene, via faecal material coming into contact with prepared carcasses; and fresh produce irrigated with contaminated irrigation water, water run-off from animal-grazed fields, or simply by wild animals traversing crop fields. Additionally, it is recognised that poor hygiene during food preparation (through direct or indirect contact between raw and final product) can lead to a range of ready-to-eat foods, such as cooked sliced meats, causing outbreaks.
Over December 2023, there were a number of recalls, beginning on Christmas Eve, of Lancashire cheese products because of possible contamination with Shiga toxin-producing E. coli. From July to December 2023, around 30 confirmed cases of STEC serotype O145 were reported across England and Scotland.
In June 2024, recalls of various prepacked, ready-to-eat sandwiches, wraps and salads were announced due to possible contamination with E. coli.
How can STEC be controlled?
Perhaps surprisingly, STEC are not that difficult to control. A standard cooking process that achieves a core temperature of 70°C for 2 minutes (or equivalent) will produce a substantial six log reduction. STEC have a similar resistance to sanitisers as that of other enteric pathogens, and their growth is considerably inhibited at chilled temperature. However, it is vitally important that the process controls used to assure safety with respect to STEC E.coli have been properly validated and shown to be effective.
Cross-contamination between raw and cooked foods can be controlled using simple hygiene measures and FSA guidance is available for food businesses to control this contamination risk. Hygiene is, similarly, a key control for preventing dairy / milking contamination in the production of milk and dairy products. The best control in fresh produce is via hygienic growth / harvesting and careful use of irrigation waters.
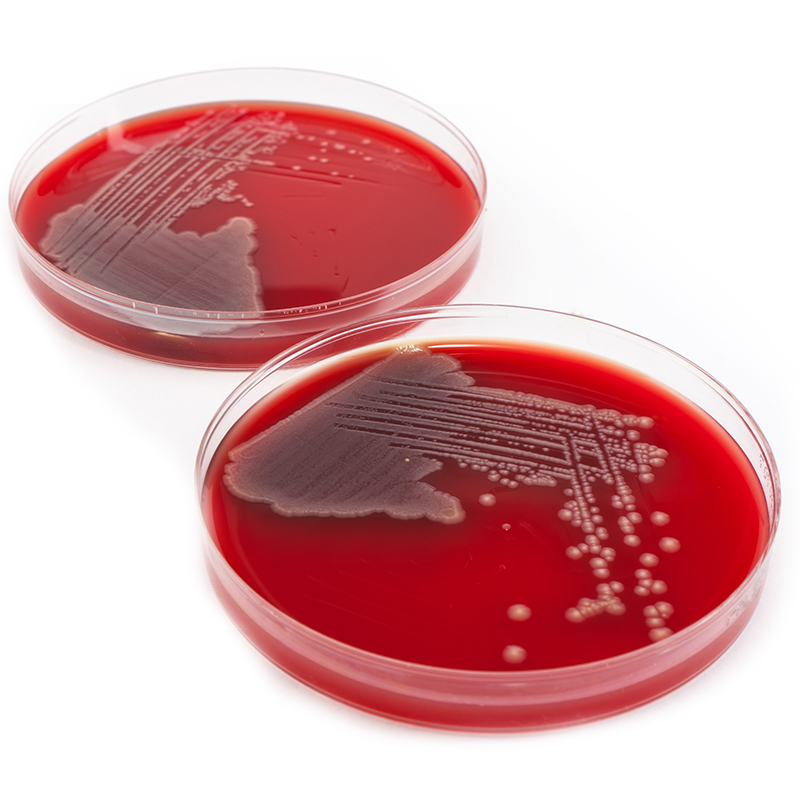
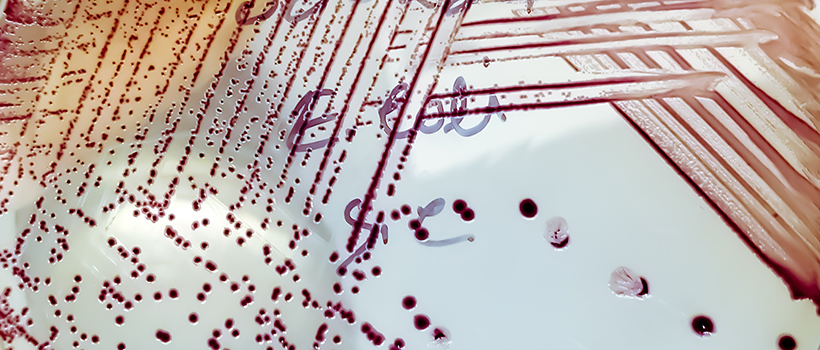
To monitor and verify the efficacy of control measures, sample analysis for STEC is usually performed. In Europe, STEC can only be handled within a Containment Level 3 pathogen laboratory, which creates challenges for method validation in many laboratories. ISO Technical Specification 13136 details a method for STEC detection in foods and we are accredited to ISO 17025 to perform this testing.
STEC analysis does not provide a simple yes/no answer, and data interpretation can be problematic. The test shows the presence of stx genes, eae genes and will report the presence of one of the top six serogroups. One of the key challenges faced by food businesses is in the interpretation of results to inform food safety decisions. Possible food safety questions that the results could raise are; what happens if one of the top serogroups is detected but the stx genes are absent? Or if the organism is not one of the named STEC serotypes but contains stx genes and could it still be a risk to consumers?
There is therefore a need to seek expert food microbiological assistance to help in interpretation and decision making.
We are here to help
Contact our experts for help with the food safety assurance of your end-to-end supply chain, including microbiology support, product testing, hygiene consultancy, process control, decontamination methods, food safety and quality management systems, incident management, root cause analysis and more.
For existing products, product development and exploring new ingredient / product categories and manufacturing processes, we can help with product microbiological risk assessment and advise on optimal risk reduction strategies.
We can advise on your testing and methodology requirements for your specific situation and product, and can conduct microbiological testing, either for routine analysis, or analysis in response to a challenge or for investigations / troubleshooting.
When it comes to hygiene and preventing contamination from the food processing / production environment, we can support with hygienic design, cleaning and environmental monitoring plans (EMP). We can visit your site to provide practical support with proactive initiatives and troubleshooting alike.
For pathogens of concern, we develop, validate and help implement effective decontamination methods into client facilities. We also support clients with process control design / review, implementation and validation – from a microbiological / decontamination perspective and more broadly.

About Suzanne Jordan
Suzanne has worked here at Campden BRI since 2005, following nine years of PhD and postdoctoral research experience in food microbiology and molecular biology of food microorganisms.
Suzanne is the lead for third party microbiological method validation studies for AOAC, MicroVal and NordVal, is a Retailer-approved Method Review Co-ordinator, and is involved in several research and contract projects for developing and evaluating new methodology. Alongside this, she is an industrial PhD supervisor for a project on the of fine-tuning dietary fibre to target gut microbiota accessibility.
During her career to date she has participated in multidisciplinary research projects involving European partners, developed expertise in a range of molecular techniques, and presented her research at an international level and in peer-reviewed journals.
How can we help you?
If you’d like to find out more about managing pathogens, contact our support team to find out how we can help
Submit samples
Visit our ‘microbiological analysis and testing’ page to find out more about testing, and to submit samples.







